Diabetes affects blood sugar, but it can also quietly harm your vision. The worst of the debilitating threats is diabetic macular edema (DME), a form of diabetic retinopathy, which can severely ruin eyesight if not caught and treated early. It’s more common than people know, affecting nearly 4% of American diabetic patients and many more around the world.
Let us discuss step by step what DME is, how it occurs, and the new ways of diagnosing and treating this condition, especially with the growing trend offered by modern ophthalmological clinics such as Dr. Natasha Lim Eye Centre in Singapore.
What is Diabetic Macular Edema
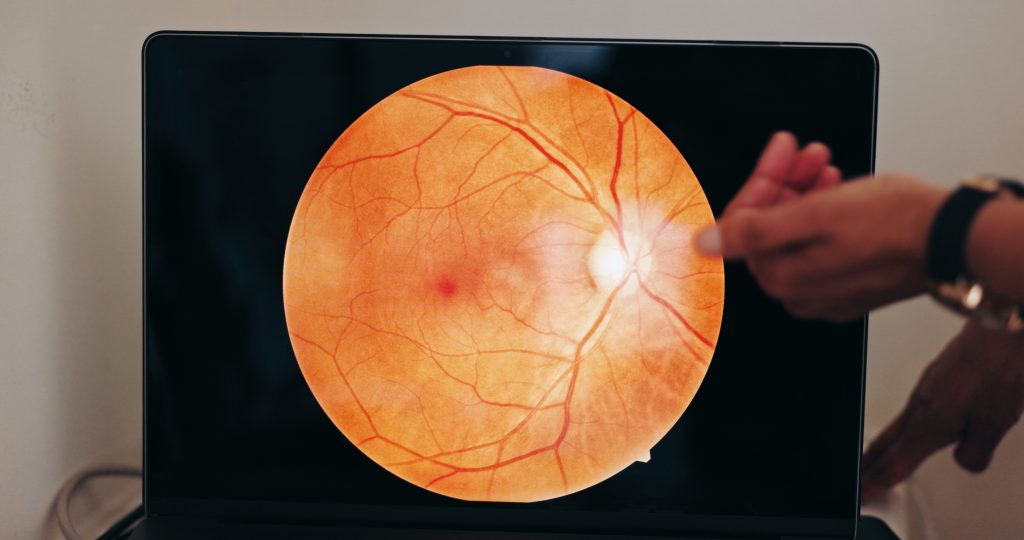
Hands, eye scan and screen in optometry for doctor, consultation and examination for vision health
Alright, so diabetic macular edema, let’s just call it DME. If your blood sugar’s running wild for too long (high blood sugar level), it damages the tiny blood vessels in your retina. They get leaky, and fluid starts pooling in the macula (that’s the bit of your eye you use to see things clearly, like when you’re reading or trying to recognize someone across the room).
So, what happens? Your vision gets all blurry. Words on a page might blur together, faces might look fuzzy, and good luck driving safely if it gets bad. Ignore DME and, yeah, you’re flirting with permanent vision loss. Not something you want to leave on your “I’ll deal with it later” list.
How DME Shows Up
Alright, so here’s the scoop: DME (Diabetic Macular Edema) doesn’t just pop up out of nowhere. It’s a messy side effect of diabetic retinopathy, think of it as diabetes’s way of pulling a fast one on your eyeballs. As blood sugar level stays high and unhinged, those tiny blood vessels in your retina start acting up, they get leaky, weak, just straight-up unreliable. Next thing you know, your body’s freaking out with inflammation and stress, and this troublemaker called VEGF (vascular endothelial growth factor) shows up, telling your blood vessels to leak even more.
So, what’s stirring the pot here? Two main culprits:
- Ischemic Retina: If your retina is not getting enough blood, it becomes oxygen-deprived and pumps out more VEGF.
- Inflammatory Damage: Diabetes keeps poking at your immune system, which messes up the barrier that’s supposed to protect your retina. More leaking. More problems.
All that nonsense leaves you with little pockets of fluid in your retina. Doctors spot these on fancy scans like OCT (Optical Coherence Tomography).
How Do You Even Know If You Have DME?

Honestly, DME is pretty sneaky. It can develop silently. You might not notice anything at all until it’s already causing trouble. That’s why regular eye checks are a big deal for anyone with diabetes. Yes, even if you think you’re fine.
Who’s on the “Get Your Eyes Checked” List?
- Type 1 diabetics: Wait about 5 years after your diagnosis, then start getting screened.
- Type 2 diabetics: No waiting, get checked out as soon as you’re diagnosed.
And don’t just make it a one-and-done thing. Yearly check-ups are the bare minimum, and if your eyes are already starting to act up, you’ll probably need to go in more often. Yeah, it’s a hassle, but so is losing your vision, honestly.

Key Diagnostics Tools
- Optical Coherence Tomography (OCT): Sounds super fancy, huh? It’s this painless scan that gives a cross-section view of your retina, layer by layer. It’s like the MRI for your eyeball, catching any sneaky fluid buildup.
- Retinal Photography: Sometimes they dilate your eyes (you know, those weird drops that make you look like an anime character), sometimes not. Either way, they snap pics to spot leaks or those little yellowish blobs (exudates, if you’re feeling technical).
- AI-Assisted Gadgets: You can find this at clinics like Dr. Natasha Lim Eye Centre. This tends to complement state-of-the-art imaging with smart diagnostic software to detect faint signs of retina changes in the initial phases. Gotta love a robot with a medical degree, right?
How Doctors Classify DME
So, doctors sort diabetic macular edema (DME) into three buckets, mostly based on how much the swelling is crashing the party near the center of your macula (that’s the spot that handles your sharp vision):
1. Mild: Swelling is not even near the main action. It’s away from the centre.
2. Moderate: Swelling’s creeping up close, but the center is still holding strong.
3. Severe: Uh oh, swelling has crashed the center, cue vision problems. Not great.
Macular Edema Treatment: What’s Working in 2025?
Diabetic macular edema has come a long way from the old days. Only a few decades ago, laser photocoagulation was the norm. Today, treatments are much more effective and often vision-restoring.
1. Anti-VEGF Injections
These are now the first-line therapy in the majority of patients. Medications like ranibizumab, aflibercept, and bevacizumab are injected directly into the eye to block VEGF, reduce leakage, and improve vision.
Clinical trials have demonstrated:
- Ranibizumab and aflibercept are recommended for those with advanced vision loss (20/50 or worse).
- Either of the three anti-VEGF drugs may be used in fewer cases.
Monthly injections are administered in most patients, with less-frequent dosing once the swelling resolves.
2. Corticosteroid Implants
In non-responders to anti-VEGF treatment (around 40% of patients), a second option is steroid implants like dexamethasone. These reduce inflammation in the retina but can cause side effects like raised eye pressure or cataracts.
Protocol U and MEAD trials both indicated that steroids do reduce swelling but aren’t always as effective at restoring vision as anti-VEGF drugs, so they are normally reserved for use.
3. Laser Photocoagulation
Although no longer the treatment of first choice, laser therapy is still useful in patients with localized inflammation or those who cannot undergo injection therapy often. It is particularly useful as an adjuvant to other therapies.
Prevention: Your Best Bet
Yeah, treatments have come a long way, but let’s be real, nothing beats just not getting the problem in the first place. If you want to keep your eyesight sharp, here’s the game plan:
- Keep your blood sugar in check. Like, check it, not just when you remember.
- Don’t sleep on blood pressure or cholesterol, either. Those sneaky little numbers can trash your blood vessels if you’re not paying attention.
- And please, go get your eyes checked. Waiting for symptoms? Bad move.
Catch issues early, and, honestly, you might never have to mess with eye injections or lasers. Vision’s one thing you don’t want to gamble with.
Wrapping Up
Diabetic Macular Edema? Yeah, it’s one of diabetes’s nastier surprises when it comes to your vision. But here’s the upside: if you spot it early, you’ve got a real shot at keeping your sight. Technology is not messing around, and the treatments now are light years ahead of where they used to be.
If you (or your friend, or your grandma, whoever) have diabetes, put eye checks on your to-do list. Regular screenings, especially at solid clinics like Dr. Natasha Lim Eye Centre, honestly could be the difference between catching something early or, well, wishing you had. Don’t wait until things get blurry.
 Tasselline | Latest Articles By Singaporeans, for Singaporeans Article Site for Singaporeans
Tasselline | Latest Articles By Singaporeans, for Singaporeans Article Site for Singaporeans